Introduction: Sickle cell disease (SCD) is debilitating and affects millions of people worldwide. Although SCD is caused by a single-point mutation of the β-globin chain of hemoglobin, the clinical manifestations are heterogeneous, and there is a lack of well-characterized predictive biomarkers of disease progression. Metabolomics is a promising tool to interrogate disease pathophysiology and underlying molecular mechanisms. Although prior metabolomic studies have been performed on human and murine red blood cells (RBCs) in the context of SCD, no systematic investigation across commonly used mouse models of SCD has been published. In the present study, we examined the blood cell metabolome of 2 widely used SCD mouse models to study and compare the metabolomic changes in disease models.
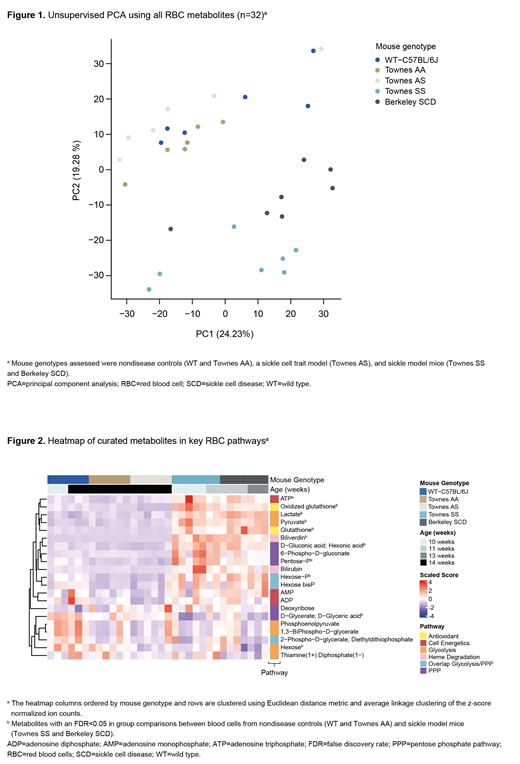
Methods: Blood samples were collected from 5 groups of mice (10-14 weeks old, n=6-7 per group): wild-type (WT) C57BL/6J mice; Townes AA, AS, and SS mice; and Berkeley SCD mice. Direct injection high-resolution mass spectrometry was used to generate untargeted metabolomics data. Three matrices (RBC, plasma, and whole blood) were isolated from each mouse group. The RBC fraction, containing peripheral blood mononuclear cells, was separated from plasma via centrifugation of whole blood. The current study focuses on the RBC dataset.Raw profile data were centroided, merged, and recalibrated using methods previously described (Fuhrer et al. Anal Chem 2011). Putative annotations were generated based on compounds contained in the Human Metabolome Database, KEGG, and ChEBI databases using accurate mass per charge (tolerance 0.001 m/z) and isotopic correlation patterns. Z-score normalization was applied across all samples for unsupervised clustering using principal component analysis (PCA) and to identify metabolites with significant changes between groups. Metabolites were mapped to central RBC metabolic pathways using MetaboAnalyst (Xia et al. Nat Protoc 2011) and manual curation.
Results: Unsupervised PCA that used all detectable RBC metabolites resulted in clear separation of mouse groups by disease status (Figure 1), suggesting robust metabolomic changes in mouse models of SCD. Focusing on the top divergent metabolites across the mouse groups, several enriched pathways were identified, such as amino acid metabolism, pyrimidine and purine metabolism, and aminoacyl-tRNA biosynthesis, all potentially attributable to the buildup of RBC precursors. Metabolites characteristic of immature RBCs were further examined, with elevated hexokinase activity (hexose:hexose-6-phosphate ratio), ATP levels, and mitochondrial metabolites found in RBCs from SCD, in line with the significantly elevated reticulocyte content in SCD mice. Metabolites were curated from additional relevant RBC metabolic pathways; some showed significant differences among mouse groups, and others were significantly elevated in sickle mice (Townes SS and Berkeley SCD) compared with non-SCD controls (WT and Townes AA), including some glycolytic and pentose phosphate pathway (PPP) intermediates (Figure 2). The product-to-substrate ratios of metabolite levels from glycolytic and oxidative PPP (oxPPP) steps suggested glycolysis was favored and the later stage of the oxPPP was reduced in mouse models of SCD. There was also a higher metabolic turnover of glutathione, which is characteristic of SCD in humans, but we observed divergent metabolomic signatures between the disease models in our study (Figure 2).
Conclusions: To our knowledge, this is the most comprehensive metabolomics study in mouse models of SCD. It provides a foundation to assess disease biology and response to treatment in future studies. Untargeted RBC metabolomics revealed metabolomic signatures that are consistent with human disease pathology in both murine SCD models, including reticulocytosis, hemolysis, and mitochondria retention in RBCs, and signatures that are unique to the murine models. Of the 2 main RBC metabolic pathways, glycolysis was favored over the oxPPP in SCD mice. This is the first step towards understanding the impact of SCD on RBC carbohydrate metabolism.
Disclosures
Montllor-Albalate:Pfizer: Current Employment. Potdar:Pfizer: Current Employment. Chen:Pfizer: Current Employment. DeGuzman:Pfizer Inc: Current Employment. Yu:Pfizer: Current Employment.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal